Polycystic Ovary Syndrome (PCOS) is not just a physical health condition; it’s a complex journey that intertwines deeply with mental health. The prevalence of PCOS is significant, affecting millions of women globally, yet its impact on mental health often remains an untold story. In a world where physical symptoms take center stage, the emotional and psychological battles women with PCOS face tend to be overlooked. This article highlights this less-discussed aspect, challenging conventional thinking and provoking a new perspective.
PCOS is commonly characterized by hormonal imbalances and metabolism issues, leading to a variety of symptoms such as irregular menstrual cycles, weight gain, acne, and fertility issues. However, the narrative seldom extends to the mental health challenges accompanying these symptoms. Women with PCOS are often on a constant battlefront, not just with their physical symptoms but with the psychological toll they take. This dual struggle can lead to feelings of isolation, anxiety, and depression, yet these mental health concerns are frequently under-acknowledged and under-treated.

The purpose of this article is to break the silence surrounding the mental health implications of PCOS. We aim to provide a more holistic understanding of PCOS by exploring the emotional and psychological impacts. This includes delving into how the symptoms of PCOS can trigger mental health issues, the role of societal stigma, and the importance of mental health awareness within the PCOS community. We will also discuss practical coping mechanisms and the significance of support systems. This article is a call to action, urging a broader conversation that includes mental health as a critical component of PCOS management. It’s about empowering women to seek help, share their stories, and find solace in knowing they are not alone in their journey.
Understanding PCOS
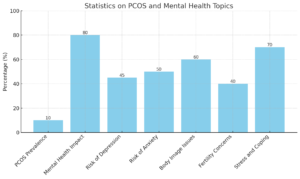
Polycystic Ovary Syndrome (PCOS) is a health puzzle wrapped in complexity and often misunderstood, even by those who experience it. As a hormonal disorder, PCOS affects approximately 1 in 10 women of childbearing age, making it a common but often underdiagnosed condition. This section aims to demystify PCOS, shedding light on its symptoms, physical implications, and the common misconceptions surrounding it, especially in the context of women seeking knowledge and support.
What is PCOS?
PCOS is a condition characterized by an imbalance in reproductive hormones. This imbalance creates problems in the ovaries, affecting ovulation and leading to irregular menstrual cycles. But PCOS is more than just a reproductive issue; it’s a complex syndrome with a spectrum of symptoms affecting various aspects of health.
Common Symptoms and Physical Implications
Women with PCOS experience a range of symptoms, and no two cases are exactly alike. The diversity in symptoms often leads to delays in diagnosis and confusion. Some of the most common symptoms include:
- Irregular Periods: This is the most common symptom, characterized by infrequent, irregular, or prolonged menstrual cycles.
- Excess Androgen: Elevated levels of male hormones may result in physical signs such as facial and body hair (hirsutism), severe acne, and male-pattern baldness.
- Polycystic Ovaries: Enlarged ovaries containing numerous small fluid-filled sacs (follicles) surrounding the eggs.
Physical Implications of PCOS
- Weight Gain and Obesity: Many women with PCOS struggle with weight gain, and obesity can exacerbate symptoms.
- Insulin Resistance: A significant number of women with PCOS have insulin resistance, leading to an increased risk of developing type 2 diabetes.
- Fertility Issues: PCOS is one of the leading causes of infertility due to irregular ovulation or failure to ovulate.
- Skin and Hair Changes: Acne, oily skin, and dandruff are common, as are skin tags and darkened patches of skin.
- Sleep Issues: Problems like sleep apnea are more common in women with PCOS.
PCOS Diagnosis and Misconceptions
Diagnosing PCOS can be challenging. There’s no single test for PCOS; instead, doctors must rule out other possible causes of the symptoms. Diagnosis typically involves a combination of physical exams, medical history, blood tests, and ultrasound.
One of the biggest misconceptions about PCOS is that it only affects overweight or obese women. While weight can influence symptoms, PCOS affects women of all body types. Another misconception is that PCOS is solely a fertility issue. While it can affect fertility, PCOS is a lifelong condition with implications for overall health, not just reproduction. Additionally, there’s a myth that PCOS symptoms disappear after menopause. In reality, while some symptoms may improve, the risk of health issues related to PCOS remains.
Understanding PCOS requires peeling back layers of complexity and addressing the diverse experiences of women who live with this condition. By doing so, we empower women with accurate information, enabling them to advocate for their health and well-being effectively. This foundation of understanding is crucial in our journey to explore the intricate connection between PCOS and mental health.

Mental Health and PCOS: The Unseen Connection
In the labyrinth of PCOS, a critical aspect often lurks in the shadows: the impact on mental health. This section delves into the psychological landscape of PCOS, illuminating the often invisible connection between this hormonal disorder and mental well-being. Women with PCOS navigate not only physical challenges but also a complex emotional terrain that deserves attention and understanding.
The Psychological Impact of PCOS Symptoms
The symptoms of PCOS are not just physical markers; they carry a psychological weight. Dealing with issues like hirsutism, acne, weight gain, and fertility concerns can significantly affect self-esteem and body image. This impact is deepened by societal pressures and the often unspoken emotional toll of living with a chronic condition. Women with PCOS frequently report feelings of shame, frustration, and isolation stemming from both the visible and invisible symptoms of the disorder.
The Stigma Associated with PCOS and its Effect on Mental Health
Stigma plays a pivotal role in the mental health challenges associated with PCOS. This stigma is twofold: the societal stigma around visible symptoms like weight and hair growth and the internalized stigma of feeling “different” or “abnormal.” The silence and misconceptions surrounding PCOS only exacerbate this issue, leaving many women feeling misunderstood and alone in their struggles.
How PCOS Affects Mental Health
- Increased Risk of Depression and Anxiety: Women with PCOS are more likely to experience depression and anxiety, often stemming from the stress of managing chronic symptoms and societal perceptions.
- Body Image Issues: Physical changes such as weight gain and hirsutism can lead to negative body image and low self-esteem.
- Emotional Turmoil from Fertility Concerns: Struggles with fertility can evoke feelings of inadequacy and grief, impacting emotional well-being.
- Social Isolation: The misunderstanding and lack of awareness about PCOS can lead to social isolation, exacerbating mental health issues.
- Stress and Coping: Chronic stress from managing PCOS and its symptoms can affect mental health, leading to a need for effective coping strategies.
Real-Life Stories and Experiences
The power of shared experiences cannot be underestimated. By bringing forward real-life stories of women battling PCOS and its mental health implications, we not only validate their experiences but also build a supportive community. These narratives reveal the resilience and strength of women facing PCOS, offering hope and solidarity to others on similar journeys.
The connection between mental health and PCOS is crucial in providing holistic care and support for women with this condition. It’s about looking beyond the physical symptoms and acknowledging the emotional and psychological battles that are an integral part of the PCOS journey. By shining a light on this unseen connection, we aim to break down barriers, reduce stigma, and foster a more compassionate and informed approach to PCOS management.
Scientific Insights: PCOS and Mental Health Disorders
As we delve deeper into the complexities of Polycystic Ovary Syndrome (PCOS), it becomes evident that the interplay between PCOS and mental health is not just anecdotal but is also backed by scientific research. This section seeks to illuminate the empirical evidence linking PCOS to various mental health disorders, offering a scientific perspective to our understanding of this intricate relationship. The insights presented here are crucial for women with PCOS, as they validate their experiences and provide a foundation for seeking appropriate care and support.
Research Findings Linking PCOS to Mental Health Disorders
A growing body of research indicates a higher prevalence of mental health disorders among women with PCOS compared to the general population. These studies provide valuable insights into how hormonal imbalances and PCOS-related symptoms can contribute to mental health challenges.
Hormonal Imbalances and Their Psychological Effects
The hormonal fluctuations characteristic of PCOS play a significant role in mental health. Hormones like estrogen and testosterone, which are often imbalanced in PCOS, have been linked to mood regulation. Additionally, insulin resistance, another common aspect of PCOS, is associated with mood disorders.
Mental Health Disorders Linked to PCOS
- Depression: Studies show a higher incidence of depression in women with PCOS, often related to the stress of chronic symptom management and hormonal imbalances.
- Anxiety Disorders: Women with PCOS are at an increased risk for anxiety disorders, including generalized anxiety and panic disorders.
- Mood Swings and Bipolar Disorder: The hormonal imbalances in PCOS can lead to significant mood swings and, in some cases, contribute to the development of bipolar disorder.
- Eating Disorders: The body image issues and weight management challenges in PCOS can increase the risk of eating disorders like binge eating and bulimia.
- Obsessive-Compulsive Disorder (OCD): There is emerging evidence linking PCOS to a higher prevalence of OCD, though the connection requires further research.
Discussing Anxiety, Depression, and Mood Swings
Anxiety and depression are the most commonly reported mental health issues among women with PCOS. The chronic nature of PCOS, coupled with societal pressures and the physical and emotional burden of the symptoms, creates a fertile ground for these conditions. Mood swings, often a direct result of hormonal fluctuations, can significantly impact daily life and relationships, adding another layer to the mental health challenges faced by these women.
The scientific insights into the connection between PCOS and mental health disorders provide a crucial lens through which to view and address the condition. Understanding the biological and psychological underpinnings of these mental health issues is key to developing effective treatment plans and support systems. This knowledge empowers women with PCOS to advocate for comprehensive care that addresses both their physical and mental health needs.

Coping Mechanisms and Support Systems
Living with PCOS is a journey that often requires navigating a complex maze of emotional and physical challenges. However, effective coping mechanisms and robust support systems can significantly ease this journey, offering solace and strength. In this section, we explore various strategies and support avenues that can help women with PCOS manage their mental health effectively. This guidance is not just about alleviating symptoms but about empowering women to lead fulfilling lives despite the challenges of PCOS.
Strategies for Managing Mental Health with PCOS
Effective management of mental health in the context of PCOS involves a combination of self-care practices, lifestyle modifications, and professional support. These strategies are aimed at not only mitigating the symptoms of PCOS but also at enhancing overall well-being.
The Role of Support Groups and Therapy
Support groups and therapy play a crucial role in the mental health journey of women with PCOS. These platforms offer a safe space to share experiences, gain insights, and receive emotional support. Therapy, particularly with professionals who understand PCOS, can be invaluable in addressing specific mental health challenges and developing personalized coping strategies.
Coping Mechanisms and Support
- Healthy Lifestyle Choices: Regular exercise, a balanced diet, and adequate sleep can help manage PCOS symptoms and improve mental health.
- Mindfulness and Stress Reduction: Techniques like meditation, yoga, and mindfulness can reduce stress and anxiety levels, promoting mental calmness.
- Building a Support Network: Connecting with friends, family, and fellow PCOS sufferers can provide emotional support and reduce feelings of isolation.
- Professional Counseling: Seeking help from mental health professionals, especially those familiar with PCOS, can provide tailored strategies for coping with anxiety, depression, and other mental health issues.
- Educational Resources: Understanding PCOS and its implications can empower women to make informed decisions about their health and treatment options.
- Hobbies and Creative Outlets: Engaging in hobbies or creative activities can provide an emotional outlet and a sense of accomplishment.
Lifestyle Adjustments for Mental Wellness
Lifestyle adjustments play a crucial role in managing both the physical and mental aspects of PCOS. These adjustments include dietary changes to manage weight and insulin resistance, regular physical activity to improve mood and energy levels, and adequate sleep to reduce stress and hormonal imbalances. Integrating these lifestyle changes into daily routines can profoundly impact overall well-being.
Coping with PCOS is a multifaceted endeavor that requires a holistic approach. By incorporating a mix of self-care practices, lifestyle changes, and professional support, women with PCOS can not only manage their symptoms but also improve their quality of life. This section aims to offer practical, actionable advice that resonates with the daily realities of women battling PCOS, empowering them to take control of their health and well-being.
Breaking the Silence: Raising Awareness and Understanding
In the discourse surrounding Polycystic Ovary Syndrome (PCOS), there’s a critical need to amplify the conversation about its impact on mental health. This section, “Breaking the Silence: Raising Awareness and Understanding,” is dedicated to fostering a greater understanding of PCOS, particularly its mental health aspects, and advocating for more open, informed discussions. For women grappling with PCOS, awareness is not just about recognizing symptoms; it’s about understanding the full spectrum of the condition, including its psychological impact.
The Importance of Talking About Mental Health in the PCOS Community
The journey of women with PCOS is often marked by silence – silence about the struggles, the emotional turmoil, and the mental health challenges they face. Breaking this silence is imperative. Open conversations about mental health in the context of PCOS can lead to better understanding, reduce stigma, and pave the way for more comprehensive care and support.
How Increased Awareness Can Lead to Better Support and Treatment
Awareness is a powerful tool. It can transform the way PCOS is perceived, treated, and managed. Increased awareness among healthcare providers, patients, and the general public can lead to earlier diagnosis, more effective treatment plans, and a more empathetic approach to care.
Steps Towards Increased Awareness and Understanding
- Educational Initiatives: Implementing educational programs and resources to inform about PCOS and its mental health implications.
- Community Outreach: Engaging in community events and social media campaigns to spread awareness and encourage open dialogues.
- Advocacy and Policy Change: Advocating for policy changes that support research and better healthcare for women with PCOS.
- Collaboration with Mental Health Experts: Collaborating with mental health professionals to develop comprehensive care plans that address both physical and mental health aspects of PCOS.
- Sharing Personal Stories: Encouraging women with PCOS to share their stories to foster a sense of community and solidarity.
- Healthcare Professional Training: Training healthcare providers to recognize and address the mental health aspects of PCOS.
Encouraging Open Discussions and Removing the Stigma
Open discussions about PCOS and mental health are essential in dismantling the stigma surrounding this condition. By talking openly about their experiences, women with PCOS can challenge misconceptions, educate others, and advocate for themselves. These discussions should extend beyond patient circles to include healthcare providers, family members, and the broader community.
Breaking the silence around PCOS and mental health is a vital step toward fostering a supportive, informed, and empathetic environment for women with this condition. This section aims to raise awareness and inspire action, encouraging all stakeholders – from patients to healthcare professionals – to engage in meaningful conversations and initiatives that can bring about tangible change. It’s about creating a world where the mental health implications of PCOS are recognized, understood, and adequately addressed, paving the way for a better quality of life for women with PCOS.
Conclusion
As we conclude our exploration of the multifaceted relationship between Polycystic Ovary Syndrome (PCOS) and mental health, it’s crucial to reflect on the key insights we’ve gathered. This journey through the various aspects of PCOS has revealed the profound impact it can have on mental well-being, the importance of understanding and managing these effects, and the power of awareness and community support. It’s evident that dealing with PCOS is more than a physical challenge; it’s a holistic battle that encompasses both the body and the mind.
For those seeking further mental health support, reputable resources are available online. Websites such as Psychology Today and Mental Health America offer directories where you can find mental health professionals and valuable information on managing mental health. These resources can be instrumental in finding the right support and understanding more about mental health in the context of PCOS.
In addition to these resources, I highly recommend the PCOS Prompt Journal on our website, All About PCOS. This journal is specifically designed to benefit women with PCOS in numerous ways:
- Encourages Reflection: The journal prompts guide you through self-reflection, helping you to understand and articulate your feelings and experiences.
- Promotes Mindfulness: Regular journaling can be a form of mindfulness practice, providing a space for calm and focused introspection.
- Aids in Stress Management: Writing about your challenges and victories can be a therapeutic way to manage stress and anxiety.
- Supports Emotional Health: The journal offers a private, safe space to express emotions, contributing to emotional well-being.
As we conclude, remember that your journey with PCOS is unique, and so is your path to managing its impact on your mental health. The insights and strategies discussed in this article aim to empower you with knowledge and tools to navigate this path. Embrace the support available, engage with the PCOS community, and remember, you are not alone in this journey. Together, we can break the silence, increase understanding, and foster a supportive environment for every woman living with PCOS.